State of Indian Healthcare Pt.IV: Universal Health Accessibility for Indians
A case for what the Indian government has done over the years to bridge the gap with special feature from our guest.
This article is sixth in a series of articles titled State of Indian Healthcare where we will compile analytical reports to provide an overview of healthcare accessibility in India. The report utilises the available Indian government healthcare data to examine various aspects related to healthcare accessibility, including availability, affordability, and quality of healthcare services across different regions of the country. The findings indicate several challenges that need to be addressed to improve healthcare accessibility in India. If you want to get the final list of data sources and references for the analytics, it will be available at the end of the last article of this series.
As mentioned in earlier articles, this post features excerpts from one of my esteemed guests who is an authority in understanding India’s public health system. We take this detour to understand, given the challenges and issues highlighted in previous articles, what the Indian government’s role has been in tackling such issues. I will first highlight what we have already covered so far before providing a brief history of the government’s contribution in providing better care and briefly touch upon what is to come next.
Recap
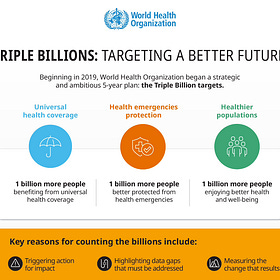
Slowly but steadily, I am building a case towards universal health coverage, not just in terms of financing options but in terms of healthcare accessibility. This is what it is all about.

In terms of financing, this is what the problem approximately looks like:
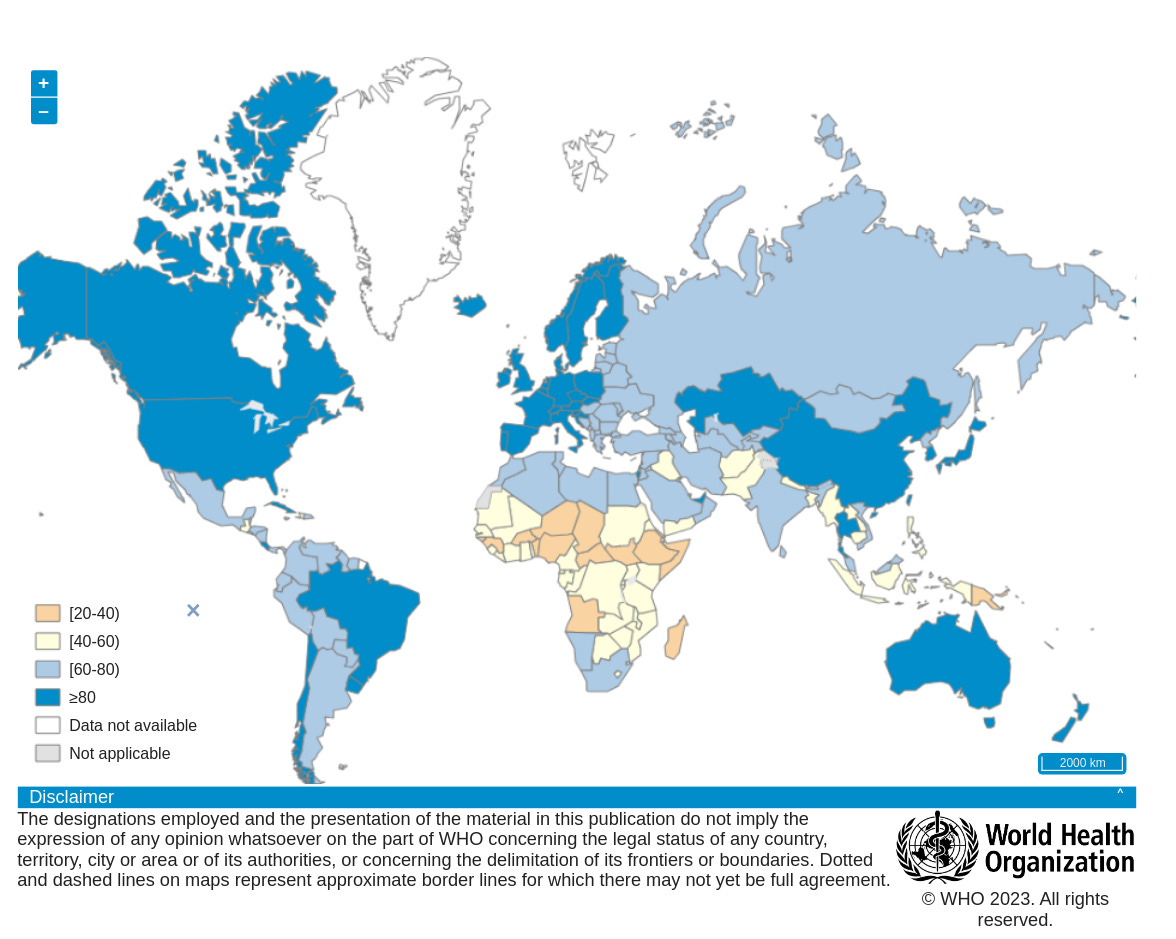
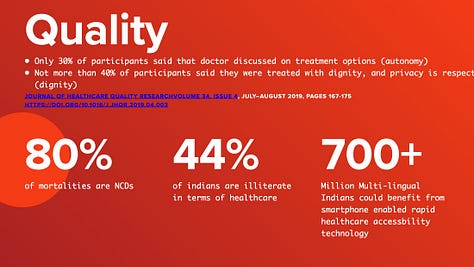
For instance, the WHO notes a lack of hospitals and clinics, poorly equipped facilities, high healthcare costs, and a high rate of non-communicable diseases. Each of these points to the multifaceted nature of the challenge – it's not just about financing healthcare but also about improving infrastructure, affordability, and preventive care.
Transforming Indian Healthcare Pt.III: A Primer on Universal Health Coverage for India
This article is fifth in a series of articles titled State of Indian Healthcare where we will compile analytical reports to provide an overview of healthcare accessibility in India. The report utilises the available Indian government healthcare data to examine various aspects related to healthcare accessibility, including availability, affordability, an…
The SCORE Assessment Summary for India can be accessed here.
In the previous article we mentioned few challenges:
Infrastructure Shortages
Under-resourced Facilities
Financial Barriers to quality care
Socio-Economic Factors
And we outlined the goals of UN SDG 3.8
We built a case for poor quality of care availability in terms of financing and accessibility as a fundamental human right. People lack awareness in India that this is a fundamental right.


Now I would like to shed some light on what the Indian government has done to solve the matters addressed in the past few articles.
A brief history of Healthcare by Indian Government
“National Rural Health Mission (NRHM) was launched in 2005 to cover the entire country with special focus on 18 States including 8 Empowered Action Group (EAG) States, viz. Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Odisha, Rajasthan, Uttarakhand, Uttar Pradesh and; 8 North Eastern States, viz. Assam, Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura, besides Himachal Pradesh and Jammu and Kashmir. NRHM was launched to provide universal access to equitable, affordable and accountable quality health care which at the same time is responsive to the needs of the people, reduction of child and maternal deaths as well as population stabilization, gender and demographic balance. It was extended to the urban areas in 2013, as the National Health Mission (NHM) with two components viz. NRHM and NUHM”, writes Dr. Bratati Banerjee.
NHM is chaired by MoHFW and is planned and executed via State Health Mission (SHM), District Health Mission (DHM) and City Health Mission (CHM) at the state, district and city levels respectively. It has four main arms:
Health system strengthening
Reproductive Maternal Newborn Child and Adolescent Health (RMNCH+A)
Communicable diseases
Non-communicable diseases
Healthcare Planning mechanism is decentralized and starts at the level of village where the VHSNC, Village Health, Sanitation and Nutrition Committee (registered society in India), prepares inter-sectoral village health plan, based on which the DPMU, the District Program Management Unit (main secretariat of the District Health Society), prepares and implements an inter-sectoral District Health Program Implementation Plan, which are then merged to form State Program Implementation Plan or State PIP.
Many of the insights from past articles that you may have read come from surveys and reports compiled by these bodies which MoHFW generously has published.
Every year Ministry of Health & Family Welfare (MOHFW) organizes the Common Review Mission (CRM) in various states across the country which assesses the status of various health programmes under NHM to understand key drivers and challenges impacting their implementation, along with documentation of innovations and best practices of each state that can be replicated elsewhere for achieving better health outcomes. Dr. Bratati adds further, “Strategies under NHM have brought about considerable improvements in the health system, particularly in the rural areas, more so with establishment of Health & Wellness Centers under Ayushman Bharat.”
Ayushman Bharat is the advent of what is now known as the Bharat Health Stack. But the roots of this mission lie in NITI Aayog which is the successor to Planning Commission in India that was setup in 1950 for planning for all sectors including health and the first Five-year Plan was launched in 1951. Within the NITI Aayog, there is a Division for Health and Family Welfare which provides policy inputs aligned to the National Health Policy 2017.
The Bharat Health Stack
Subsequently, Ayushman Bharat was launched in 2018 with two major components viz. Health and Wellness Centers (AB-HWC) and Pradhan Mantri Jan Arogya Yojana, PM-JAY. In 2019, the National Health Authority (NHA) was formed for implementing PMJAY. Thus, under NHM, NHA steers the modern national healthcare scheme, PM-JAY.
Ayushman Bharat Digital Mission (ABDM), launched in 2021 is the digital arm of Ayushman Bharat, for facilitating the provision of health services to the citizens by creating and maintaining a repository of digital records of citizens (ABHA number), record of healthcare professionals (Healthcare Professionals Registry or HPR) and healthcare facilities (Health Facilities Registry or HFR). ABDM helps to support the digitalization of health services in India, steered by the NHA.
Healthtech organizatons offering everything from tele-consultation, doctor’s appointment to medicine delivery, such as Practo, Medibuddy and the likes all target a pie in the sky of this revolutionary healthcare stack.
So in the last decade, the government has gone from planning to rebranding to launching few modern projects to integrate healthcare into the modern Bharat Stack.
When we mention digitalization of healthcare services in the context of ABDM, this stack is at its nascent phase, with each individual supposed to get an ABHA ID, which is health ID for ABDM. So how is the government, you ask, tackling the challenge of linking so many healthcare bodies across multiple tiers of its federal healthcare structure and overcoming the challenges of transforming more than 70% manually run care services into digital care centres?
Internet connectivity, hardware and software systems, digital awareness, literacy, user competency, integration and sharing of PII data in a compliant and secure manner between various systems while tackling cost and sustainability of operating the system as well as dealing with resistance to conventional methods are all the challenges yet to be overcome. Only a handful of players in the Bharat Stack vision have been able to integrate into this voluntary phase of the system at best. However, the government plans to make it mandatory for the stakeholders to use this system.
NHA developed the concept of a “Microsite” and ABDM implemented the first microsite pilot in Mumbai, Maharashtra in 2022, followed by two more in Gujarat at Ahmedabad and Surat. With the encouraging response from these pilot microsites, NHA initiated the ‘100 Microsites Project’ under ABDM in 2023 as an endeavour to promote digital health adoption and hence make healthcare more accessible to all specially in the private sector. Under this project, explains Dr. Banerjee, 100 such Microsites would be established across the country and focused efforts would be made to bring all healthcare entities under the ABDM fold.
A Microsite, within the context of ABDM, is a cluster of all small and medium scale clinics, nursing homes, hospitals, preferably <10 bedded, laboratories, pharmacies and other healthcare facilities that are ABDM-enabled and offer digital health services to the patients.
The government’s plans with National Health Missions and ABDM has been a top-down approach, something only something as powerful as a government can enforce. Pilot projects report of its transformative potential for the future, but for now, the common man still has some miles to walk until they can avail these benefits.
So, in effect, how is ABDM going to be the great enabler and solve a bigger problem for the poor India? How effective has Ayushman Bharat program been for this section of society, which forms the majority in India?
In the next article, I will invite another guest to highlight what is currently being done by private players and their involvement with ABDM and experiences in bringing the dream of healthcare accessibility closer to the common man.
To be contd…
Dr. Bratati Banerjee (WHO Fellowship in Epidemiology of Non-Communicable Diseases) is the Director Professor, Department of Community Medicine, Maulana Azad Medical College. Her publications cover over 30 papers in national and international journals and has authored books on public health policies and works in the field of epidemiology, non communicable diseases and public health management.